MedBridge and CollaborateHealth have joined forces to empower patients and healthcare providers with personalized support for successful recovery and sustained wellness.
At MedBridge Healthcare, we understand the challenges and complexities surrounding hospital readmissions.
We’ve partnered with CollaborateHealth to develop a comprehensive Hospital Readmission Reduction Program designed to empower patients and healthcare providers. Our program goes beyond traditional transitional care by offering personalized support and resources to ensure a successful recovery and long-term health.
About the Readmission Reduction Program
Reduce costs, improve outcomes, and increase quality of life for high-risk CHF, COPD, and other patients through our Readmission Reduction Program.
Components of this program include:
We Take a Patient-Centric Approach
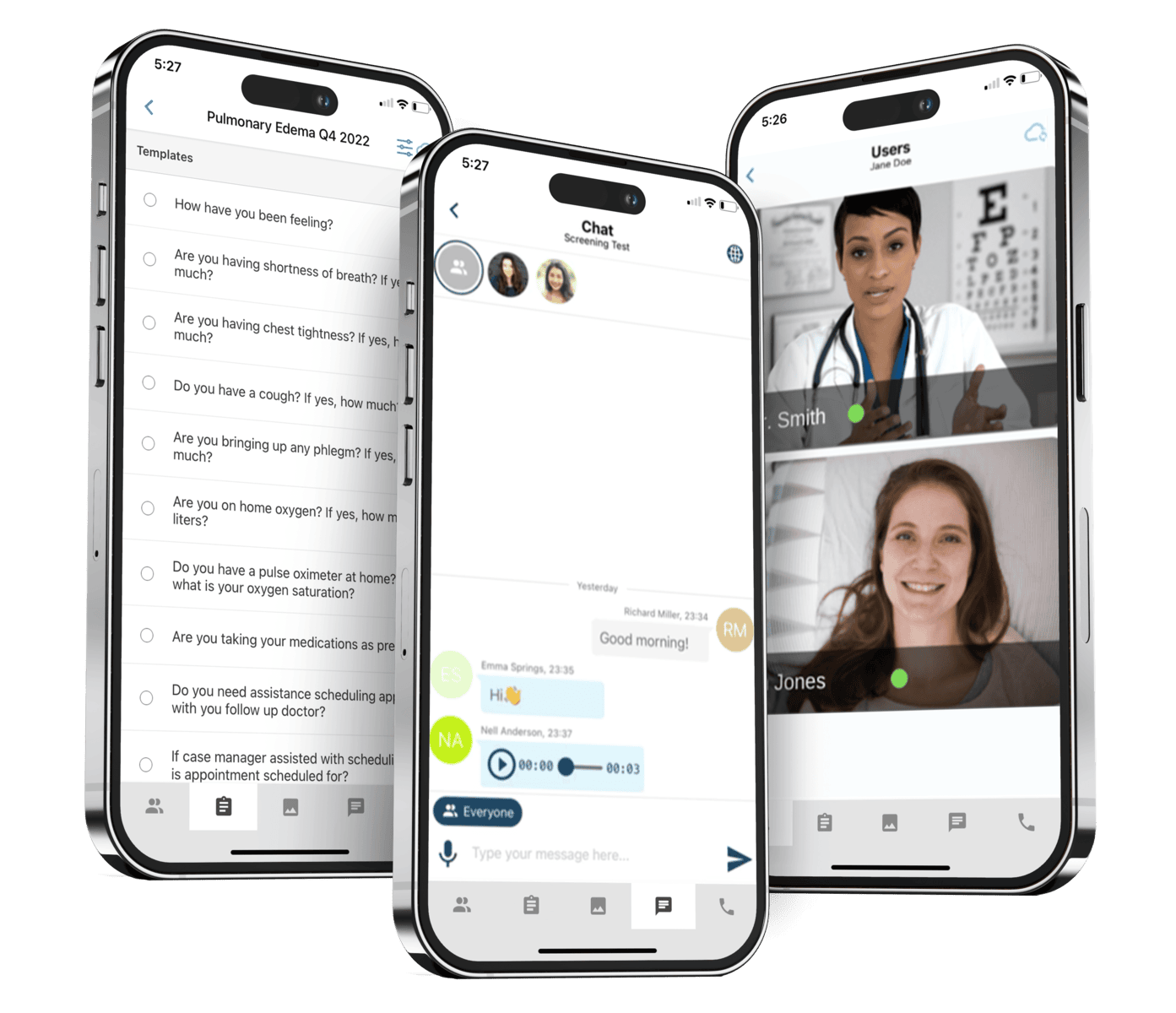
Our Readmission Reduction Program is a personal resource for patients, offering daily monitoring and check-ins, medication reconciliation, and comprehensive patient education. Pharmacists and nurses can check in daily, provide symptom checkers, and offer ongoing support after discharge.
A Platform Customized to Your Hospital's Needs
We understand that every hospital and healthcare system is unique, so our program is fully customizable to fit your needs. Whether you require an inpatient navigator, pre-discharge loaner equipment, or bedside consultations by board-certified sleep physicians, we work closely with you to tailor the program accordingly.
Our Platform is HIPPA Compliant
Our program leverages the power of remote patient monitoring to keep track of patients' health and well-being. We integrate device APIs from popular platforms to achieve this. This integration allows us to collect and analyze various health metrics such as heart rate, blood pressure, and sleep patterns.
How Our Program Works
Initial Assessment
Personalized Care Plan
Daily Support & Monitoring
Ongoing Support
Average cost per CHF readmission
1 in 5 Medicare beneficiaries is readmitted within 30 days of discharge.
Average cost per COPD readmission
A quarter of readmissions were determined to be preventable and medication-related.
Sources:
1 - Urbich M, Globe G, Pantiri K, et al. A Systematic Review of Medical Costs Associated with Heart Failure in the USA (2014-2020). Pharmacoeconomics. 2020;38(11):1219-1236. doi:10.1007/s40273-020-00952-0
2 - Scalzitti NJ, O’Connor PD, Nielsen SW, et al. Obstructive Sleep Apnea is an Independent Risk Factor for Hospital Readmission. J Clin Sleep Med.2018;14(5):753-758. Published 2018 May 15. doi:10.5664/jcsm.7098
3 - Portillo EC, Wilcox A, Seckel E, Margolis A, Montgomery J, Balasubramanian P, Abshire G, Lewis J, Hildebrand C, Mathur S, Bridges A, Kakumanu S. Reducing COPD Readmission Rates: Using a COPDCare Service During Care Transitions. Fed Pract. 2018 Nov;35(11):30-36.PMID: 30766329; PMCID: PMC6366592.
4 - https://www.japha.org/article/S1544-3191(17)30778-1/fulltext
Schedule a Demo Today
Are you ready to transform your transitional care approach and reduce hospital readmissions?
Schedule a demo of our program today! With no financial risk for hospitals to utilize the program, there’s no better time to take action and improve patient outcomes while lowering costs. Contact us now to get started.



